On this Page
- Calcium is important for your bones – and so much more
- Most Canadians are NOT getting enough calcium – it’s a real problem!
- How much calcium do you need daily?
- What you need to know about calcium and osteoporosis
- Strong bones need more than calcium – other nutrients matter too!
- Where can you find calcium?
- Serving up calcium
- Sources
Calcium is important for your bones – and so much more
You’ve probably been hearing about the calcium and bone connection for as long as you can remember. Well, there is a good reason for that – calcium is the most abundant mineral in the body, and 99% of it is stored in your bones.1
Getting enough calcium at each stage of life can help keep bones healthy by:2-6
- Supporting healthy bone growth and development during childhood.
- Building bone mass during teen years. This time of life is important as bones are still growing. Peak bone mass is typically reached for most people by age 30.
- Contributing to bone density in adulthood.
- Helping prevent osteoporosis, a disease that weakens bones and makes them more likely to break, mainly in older adults.
Calcium also has many other important functions:2, 7-11 It helps keep teeth strong and your blood flowing. It helps support muscles (including your heart) and nerve function, and it plays a key role in hormone secretion. Calcium may also play a role in reducing your risk of colorectal cancer and maintaining a healthy blood pressure.
This video was produced in 2024 using the Health Canada Canadian Nutrient File data available at the time. As a result, some figures may differ slightly from the current values presented in this article.
Calcium is important for everyone – not just for kids or older adults !
Most Canadians are NOT getting enough calcium – it’s a real problem!
On average, 68% of Canadians aren’t getting enough calcium from their diet.12 This includes:
- 42% of children (aged 1 to 8);
- 86% of teenage girls (aged 14-18);
- About 75% of women (aged 19-50);
- 91% of older male adults (aged 71 and older);
- 97% of older female adults (aged 71 and older).
Other age groups are also struggling to get enough calcium, making these low intakes of calcium a significant public health concern.12,13
Because your body cannot produce calcium on its own, you need to get it from your diet.6
How much calcium do you need daily?
Health Canada and Osteoporosis Canada recommend the following:14,15
Calcium Recommendations
| Age | Recommended Amount (mg) per day |
| 1-3 | 700 |
| 4-8 | 1,000 |
| 9-18 | 1,300* |
| 19-50 | 1,000* |
| 51-70 | 1,200 (female) 1,000 (male) |
| 71+ | 1,200 |
What you need to know about calcium and osteoporosis
Peak bone mass — when bones are at their strongest — is typically reached during young adulthood. But as a living tissue, your bones continue to change throughout your life — growing, renewing and repairing — as needed.16
When you don’t get enough calcium in your diet to maintain essential functions, your body takes what it needs out of your bones. Over time, this can cause your bones to become fragile, leading to fractures and osteoporosis.17 Osteoporosis is a disease characterized by low bone mass and deterioration of bone tissue. According to Osteoporosis Canada, at least 1 in 3 women, and 1 in 5 men, will break a bone due to osteoporosis in their lifetime.18
Osteoporosis is often referred as the “Silent Thief”.19 Since it develops slowly over many years without any obvious symptoms, you may not even realize it’s happening.
By the time bones become weak and start to break, osteoporosis may already be advanced and harder to manage. When it comes to bone health, adopting healthy lifestyle habits early on can make a difference.
- Consume a diet rich in calcium that includes other bone-building nutrients every day throughout life.
- Be physically active and include balance and strength exercises in your weekly routine.
- Limit your alcohol intake.
- Be smoke-free.20
Strong bones need more than calcium – other nutrients matter too!
While calcium plays a key part in preventing osteoporosis and keeping your bones strong, it doesn’t work alone! Osteoporosis Canada recommends adequate intakes of vitamins D and K, protein and magnesium. There are other important bone-health allies, including vitamin A and phosphorus. These nutrients, along with other compounds found in whole foods, interact and work together to support your overall health.21
When it comes to bone health, let nutritious food be your foundation, as the nutrients in food work together to support healthy bones.
Where can you find calcium?
Milk products – like milk, cheese and yogurt – are among the best natural sources of calcium. You can also find good amounts in canned fish with bones (remember: the bones are important), and smaller amounts in legumes, vegetables, nuts and seeds. Calcium-fortified foods and calcium-set tofu can also contribute to your calcium intake.
The table below shows how much calcium is found in commonly consumed foods, and indicates whether they are considered a source of calcium according to Health Canada’s criteria (providing at least 65 mg of calcium per serving).
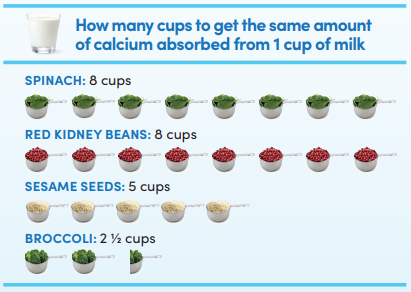
Keep in mind that the amount of calcium your body absorbs can vary. For example, calcium from milk products, broccoli, bok choy and kale is well absorbed. However, the naturally occurring calcium in many other plant-based foods is less well absorbed due to naturally present compounds in these foods that limit calcium absorption. This is particularly true for sesame seeds, spinach and rhubarb which provide valuable nutrients, but are not reliable sources of calcium. For calcium-fortified foods, the type of calcium added can also affect how well your body absorbs it.22-24
Calcium Content of Common Foods25,26
| Food | Serving Sizea | Calcium Content (mg) | Source of Calcium (≥65mg/serving) |
| Milk products | |||
| Milk (2% milk fat) | 250 mL | 309 | Yes |
| Cheddar Cheese | 30 g | 202 | Yes |
| Cottage Cheese | 125 g | 139 | Yes |
| Mozzarella Cheese | 30 g | 172 | Yes |
| Swiss Cheese | 30 g | 237 | Yes |
| Yogurt, plain (2 – 3.9% milk fat)b | 115 g | 131 – 175 | Yes |
| Yogurt, vanilla or fruit flavoured (2 – 3.9% milk fat)b | 115 g | 125 – 144 | Yes |
| Greek Yogurt, plain (2% milk fat)b | 115 g | 115 – 148 | Yes |
| Greek Yogurt, vanilla or fruit flavoured (2% milk fat)b | 115 g | 99 – 148 | Yes |
| Vegetables | |||
| Bok Choy, boiled, drained, shredded | 125 mL | 84 | Yes |
| Collards, boiled, drained, chopped | 125 mL | 142 | Yes |
| Broccoli, boiled, drained, chopped | 125 mL | 33 | No |
| Kale, boiled, drained, chopped | 125 mL | 49 | No |
| Sweet Potato, boiled, without skin, mashed | 140 g | 38 | No |
| Fruits | |||
| Orange, raw | 1 medium | 52 | No |
| Nuts and seeds | |||
| Almonds, unroasted or dry-roasted, unblanched | 30 g (60 mL) | 81 | Yes |
| Chia Seeds | 30 g (45 mL) | 189 | Yes |
| Flax Seeds | 30 g (45 mL) | 76 | Yes |
| Hemp Seeds | 30 g (45 mL) | 22 | No |
| Sesame Seeds, dried, shelled | 30 g (60 mL) | 18 | No |
| Legumes | |||
| Edamame, boiled | 125 mL | 138 | Yes |
| Navy Beans, boiled | 125 mL | 66 | Yes |
| White Beans, boiled | 125 mL | 85 | Yes |
| Hummus, commercial | 30 g (30 mL) | 11 | No |
| Pinto Beans, boiled | 125 mL | 42 | No |
| Red Kidney Beans, boiled | 125 mL | 26 | No |
| Fish | |||
| Salmon, sockeye (red), canned with bones, drained | 100 g | 239 | Yes |
| Sardines, canned with bones, drained | 100 g | 382 | Yes |
| Fortified Foods | |||
| Fortified plant-based Beverages (soy, almond, oat, cashew, etc.)c | 250 mL | 313 | Yes |
| Tofu, firm or extra-firm, prepared with calcium sulfated | 85 g | 75 – 225 | Yes |
aServing sizes for each food are based on the reference amounts from the Canadian Food Inspection Agency’s nutrition labelling requirements.
bCalcium content of yogurt varies; presented ranges are based on a 2025 Canadian marketplace scan for regular yogurts (2 – 3.9% milk fat) and Greek yogurts (2% milk fat). Check the label for more information.
cSome plant-based beverages are fortified with calcium – check the label. As per Health Canada regulations, when plant-based beverages are fortified, they must contain 125 mg of calcium per 100 ml; the table above reflects this. Keep in mind that added calcium may settle at the bottom of the container – and remain there, even after vigorous shaking – so these beverages may not be a reliable source of calcium. Also, the form of calcium used in fortification may not be as well absorbed as the naturally occurring calcium in cow’s milk. 27, 28
dCalcium content of calcium-set tofu varies considerably by brand and type; presented values are based on a 2022 Canadian marketplace scan for firm/extra firm tofu. Check the label for more information.
Serving up calcium
Getting enough calcium each day doesn’t have to be complicated. The recipes in this section show you how to easily add foods high in calcium to every meal – from breakfast through supper – so you can help keep your bones healthy, all while enjoying what you eat.
Kickstart your morning with:
Strawberry Banana Granola Breakfast Parfait | What you eat
Overnight Hearty Oatmeal Breakfast | What you eat
Refuel your body at lunchtime with:
Chicken Grilled Cheese | What you eat
Kasha Bowl with Vegetables and Chicken | What you eat
Easy Broccoli, Bean and Fusilli Pasta | What you eat
End the day strong with these suppers:
One-Skillet Creamy Chicken Rotini | What you eat
Simple Mushroom, Spinach and Tomato Frittata | What you eat
In need of more bone-building meal inspirations? Click the Recipes tab at the top of this webpage to explore our full collection of recipes.
Remember: It’s never too late, no matter your age, to take steps to add more calcium and other bone-building nutrients to your diet.
Sources
- International Osteoporosis Foundation. 2025. Calcium. www.osteoporosis.foundation.
- Institute of Medicine. 2011. Dietary Reference Intakes for Calcium and Vitamin D. Accessed September 25, 2025.
- Khemayanto, H et al. The Effects of Dairy Product Supplementation on Bone Health Indices in Children Aged 3 to 18 Years: A Meta-Analysis of Randomized Controlled Trials. Adv Nutr 2023;14:1187-1196.
- Weaver, C M et al. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporosis Int. 2016;27;1281-1386.
- Iuliano, S et al. Effect of dietary sources of calcium and protein on hip fractures and falls in older adults in residential care: cluster randomised controlled trial. BMJ. 2021. doi: 10.1136/bmj.n2364
- World Health Organization & Food and Agriculture Organization of the United Nations. Vitamin and mineral requirements in human nutrition (2nd ed.). Geneva: WHO. 2004.
- Theodoridis, X et al. Adherence to the DASH Diet and Risk of Hypertension: A Systematic Review and Meta-Analysis. Nutrients 2023. doi: 10.3390/nu15143261.
- Heart & Stroke. 2024. The DASH Diet to lower high blood pressure. www.heartandstroke.ca. Accessed September 25, 2025.
- Papier, K et al. Diet-wide analyses for risk of colorectal cancer: prospective study of 12,251 incident cases among 542,778 women in the UK. Nat Commun 2025. Doi: 10.1038/s41467-024-55219-5.
- American Institute for Cancer Research. 2020. Colorectal Cancer. www.aicr.org Accessed September 25, 2025.
- Villa-Etchegoyen, C et al. Mechanisms Involved in the Relationship between Low Calcium Intake and High Blood Pressure. Nutrients 2019. doi: 10.3390/nu11051112.
- Vatanparast, H et al. Calcium Intake from Food and Supplemental Sources Decreased in the Canadian Population from 2004 to 2015. J Nutr 2020; 150 (4); 833-841.
- Health Canada. 2016. Evidence Review for Dietary Guidance: Summary of Results and Implications for Canada’s Food Guide. Canada.ca. Accessed September 25, 2025.
- Health Canada. 2023. Dietary reference intakes tables: Reference values for elements. www.canada.ca. Accessed September 25, 2025.
- Osteoporosis Canada. 2025. Adequate Calcium Intake Can Slow Bone Loss and Reduce the Risk of Fracture. www.osteoporosis.ca. Accessed September 25, 2025.
- National Institutes of Health. 2025. Calcium: Factsheet for Health Professionals. Accessed September 25, 2025.
- Osteoporosis Canada. 2025. About the Disease. www.osteoporosis.ca. Accessed September 25, 2025.
- Osteoporosis Canada. 2022. 2022 Osteoporosis Canada Facts and Stats. www.osteoporosis.ca. Accessed September 25, 2025.
- Osteoporosis Canada. 2025. What is Osteoporosis? The Silent Thief. www.osteoporosis.ca. Accessed September 25, 2025.
- Osteoporosis Canada. 2025. Risk Factors. www.osteoporosis.ca. Accessed September 3, 2025
- Weaver, C M and Givens, D I. Overview: the food matrix and its role in the diet. Critical Reviews in Food Science and Nutrition 2025. doi: 10.1080/10408398.2025.2453074
- Weaver, C M et al. An algorithm to assess calcium bioavailability from foods. J Nutr 2024;154:921-927.
- Shkembi, B and Huppertz T. Calcium absorption from food products: food matrix effects. Nutrients 2022. doi:10.3390/nu14010180
- Heaney R P et al. Calcium fortification systems differ in bioavailability. J Am Diet Assoc. 2005;105:807–809.
- Health Canada. Canadian Nutrient File. Accessed September 25, 2025.
- Canadian Food Inspection Agency. Nutrient content claims: what they mean – www.canada.ca. Accessed September 25, 2025.
- Chalupa-Krebzdak S et al. Nutrient density and nutritional value of milk and plant-based milk alternatives. Int Dairy J 2018;87: p. 84-92.
- Rafferty K et al. Calcium fortificants: Overview and strategies for improving calcium nutriture of the U.S. population. J Food Sci 2007;72(9):R152-158.